In recent years, there has been a growing recognition of the importance of the human microbiome in regulating numerous bodily functions. Among its most critical roles is its influence on the immune system. The microbiome, which is composed of trillions of microorganisms (including bacteria, viruses, fungi, and other microbes) residing primarily in the gut, is not just a passive inhabitant of our bodies. It plays an active role in maintaining immune balance and protecting the body from disease. Microbiome diversity—the variety and abundance of different microorganisms in the body—has emerged as a key factor in determining immune health. In this article, we will explore how microbiome diversity influences immune function and why preserving this diversity is vital for human health.
The Gut Microbiome: A Central Player in Immune Regulation
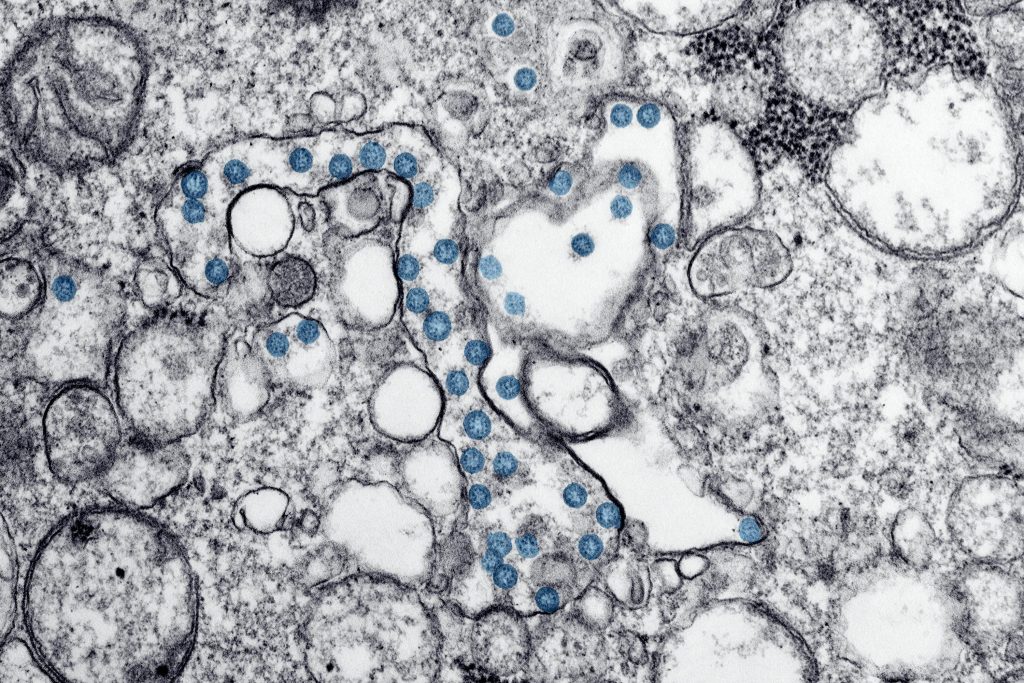
The largest and most well-studied microbiome resides in the gut, which contains around 100 trillion microbes, outnumbering human cells by 10 to 1. The gut microbiome is a dynamic ecosystem that plays an essential role in digestion, synthesizing vitamins, and metabolizing various compounds. However, its interaction with the immune system is particularly fascinating. The gut mucosa, the inner lining of the intestines, is home to about 70% of the body’s immune cells, placing it in direct contact with the microbiome. This proximity allows the gut microbiome to influence immune responses both locally and systemically.
The immune system and the gut microbiome are in a constant state of interaction. Immune cells monitor microbial populations and ensure that pathogenic (harmful) microbes do not take hold, while beneficial microbes help to train the immune system and regulate its activity. This delicate balance is essential for immune tolerance—where the immune system recognizes beneficial bacteria as friendly and does not mount an unnecessary inflammatory response.
Microbiome Diversity and Immune Function: A Complex Relationship
The diversity of the gut microbiome—the range of different microbial species present—plays a critical role in immune function. A diverse microbiome is thought to be more resilient and capable of resisting disease because it can maintain balance more effectively. In contrast, a reduction in microbiome diversity, also known as dysbiosis, has been linked to several health issues, including autoimmune diseases, allergies, and infections.
1. Immune System Maturation and Microbiome Diversity
Microbiome diversity is especially important in early life, as it is during infancy and childhood that the immune system undergoes significant maturation. When a baby is born, its immune system is relatively underdeveloped and must learn to distinguish between harmful and harmless microbes. The exposure to a diverse microbiome through birth, breastfeeding, and environmental interactions is crucial in shaping the immune system’s ability to recognize pathogens and avoid overreacting to non-threatening substances, like allergens.
Studies have shown that infants born via cesarean section, who miss out on exposure to maternal vaginal microbiota, often have less microbial diversity and are at increased risk for developing immune-related conditions such as asthma and allergies. Breastfeeding further enhances microbiome diversity by providing both beneficial bacteria and immune-modulating compounds that promote healthy immune system development.
2. Microbiome Diversity and Immune Tolerance
One of the key functions of the immune system is to distinguish between self and non-self, and to tolerate beneficial microbes while attacking pathogens. A diverse microbiome helps to “train” the immune system to recognize which microbes are beneficial and which are harmful. In the absence of this microbial diversity, the immune system may become hyper-reactive, leading to autoimmune diseases, where the immune system attacks the body’s own cells, or to allergies, where the immune system overreacts to harmless substances.
The hygiene hypothesis, which posits that the modern rise in autoimmune diseases and allergies may be linked to reduced microbial exposure during childhood, highlights the importance of microbial diversity. This theory suggests that children growing up in overly sanitized environments may not be exposed to the range of microbes necessary to develop immune tolerance, leading to an overactive immune response later in life.
3. Gut Microbiome and Immune Inflammatory Responses
The microbiome also has a direct role in regulating inflammation, a core component of the immune response. Inflammation is a natural immune response to infection or injury, but chronic inflammation can lead to a range of diseases, including autoimmune disorders, cardiovascular disease, and cancer.
A diverse microbiome helps to regulate inflammation by producing anti-inflammatory compounds, such as short-chain fatty acids (SCFAs) like butyrate, which are derived from the fermentation of dietary fibers by gut bacteria. Butyrate, in particular, has been shown to enhance the function of regulatory T cells (Tregs), a type of immune cell that helps to suppress inflammatory responses and maintain immune balance. Reduced microbiome diversity has been associated with increased levels of inflammatory markers in the body, indicating a potential pathway by which dysbiosis contributes to chronic diseases.
4. The Role of the Microbiome in Immunotherapy
Microbiome diversity may also influence the effectiveness of certain medical treatments, including immunotherapies. Immunotherapy, which is increasingly used to treat cancers such as melanoma and lung cancer, works by harnessing the body’s immune system to fight disease. Recent studies have found that patients with a more diverse gut microbiome tend to respond better to immunotherapy. Conversely, a less diverse microbiome has been linked to poorer treatment outcomes.
This connection between microbiome diversity and immunotherapy response suggests that modifying the microbiome, through diet, probiotics, or even fecal microbiota transplantation, could potentially enhance the effectiveness of these treatments. While this is still an emerging area of research, it underscores the significant role the microbiome plays in modulating immune responses.
Factors Affecting Microbiome Diversity
Several factors influence microbiome diversity, many of which are related to lifestyle and environmental exposures. Understanding these factors can help individuals and healthcare providers make informed choices to preserve or restore microbiome diversity, thereby supporting optimal immune function.
1. Diet
Diet is one of the most important determinants of microbiome diversity. A diet rich in fiber, fruits, vegetables, and fermented foods promotes the growth of diverse, beneficial bacteria. In contrast, diets high in processed foods, refined sugars, and unhealthy fats have been associated with reduced microbiome diversity and an increased risk of inflammatory diseases.
The Mediterranean diet, which is rich in fruits, vegetables, whole grains, and healthy fats, has been shown to support microbiome diversity and reduce inflammation. Conversely, the Western diet, characterized by high intakes of red meat, processed foods, and sugars, is linked to reduced diversity and higher levels of inflammatory markers.
2. Antibiotic Use
While antibiotics are life-saving drugs, they also have the potential to significantly disrupt the microbiome by killing off not only harmful bacteria but also beneficial microbes. Frequent or inappropriate antibiotic use can lead to a long-term reduction in microbiome diversity, making individuals more susceptible to infections, allergies, and autoimmune conditions. Recovery of microbiome diversity after antibiotic use can take weeks, months, or even years, and in some cases, certain bacterial populations may not recover fully.
3. Environmental Exposure
Exposure to a wide range of microbes through contact with soil, animals, and other people can help to promote microbiome diversity. Rural living, farming, and having pets have all been associated with a more diverse microbiome. On the other hand, urban living, reduced contact with nature, and excessive cleanliness may limit microbial exposure and contribute to reduced diversity.
Conclusion
The microbiome plays a pivotal role in regulating immune function, and maintaining a diverse microbiome is essential for immune health. A diverse microbiome helps to train the immune system, promote immune tolerance, regulate inflammation, and even enhance the effectiveness of immunotherapy. Factors such as diet, antibiotic use, and environmental exposure significantly influence microbiome diversity, highlighting the importance of lifestyle choices in preserving microbial balance.
As research into the microbiome and immune function continues to advance, it is becoming increasingly clear that fostering a diverse microbiome is a key strategy for maintaining overall health and preventing disease. By understanding the factors that shape microbiome diversity and making informed choices, we can support our immune system in its crucial role of protecting us from harm while maintaining balance within the body.